National Travel Week, Mental Health Month, Older Americans Month and Celebrating Moms Sherri Snelling, corporate gerontologist and “Caregiving Club On Air” podcast host, celebrates May’s Older Americans Month and National Travel Week May 7-13 with her guests for this...
Sherri Snelling
Season 3, Episode 24 – Show Notes and Resource Links
Stress Awareness Month, Companies That Care, Volunteer Week & Garden Month Sherri Snelling, corporate gerontologist and “Caregiving Club On Air” podcast host interviews on this episode: Francesca ReDavid, senior director of product growth at Care.com. Francesca...
Celebrating National Memory Day and International Happiness Day
Learn how brain health is tied to happiness through Sherri Snelling’s articles.
Season 3, Episode 23 – Show Notes and Resource Links
National Nutrition Month with Brain Health Kitchen author, International Happiness Day & Reading Nooks for Niksen Breaks Sherri Snelling, corporate gerontologist and “Caregiving Club On Air” podcast host interviews on this episode: Dr. Annie Fenn, author - Brain...
Season 3, Episode 22 – Show Notes and Resource Links
Spring Forward - Sleep Science, National Dream Day and National Color Therapy Month Sherri Snelling, corporate gerontologist and “Caregiving Club On Air” podcast host has two great guests this episode:: Kathryn Grube, CEO and Founder of Functional Color Solutions is a...
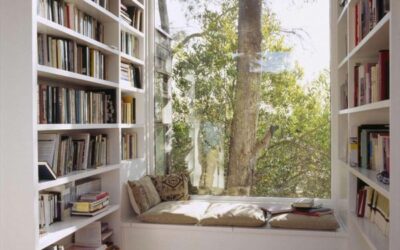
Create a Cozy Reading Nook for National Day of Unplugging – March 3
Tis the season of the digital detox as we celebrate the National Day of Unplugging on March 3. The art of unplugging is captured in two different ways by our friends in Nordic countries: the art of hygge and niksen.
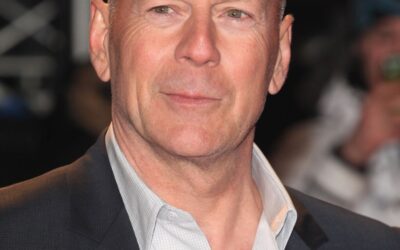
Bruce Willis Update: The “Die Hard” Star’s Dementia Diagnosis
For Father’s Day Sherri reports on Bruce Willis and what is aphasia? Plus communicating with fathers and her personal dad story.
Season 3, Episode 21 – Show Notes and Resource Links
National Caregiver Day, Soulmates & Solo Agers, Heart Health Month & Go Red for Women! Sherri Snelling, corporate gerontologist and “Caregiving Club On Air” podcast host presents our February epsiode with an expert guest interview for National Caregiver Day...
Season 3, Episode 20 – Show Notes and Resource Links
Financial Wellness Month, Harvard Study & New Book on Living Longer, Hugs for Health Sherri Snelling, corporate gerontologist and “Caregiving Club On Air” podcast host kicks off 2023 and Season 3 with a focus on January Financial Wellness Month and a time...
Season 2, Episode 19 – Show Notes and Resource Links
HOLIDAY Episode: The Five Wishes, Holiday Shopping with Journey Health & Lifestyle and our 2nd Annual Caregiver Holiday Gift Guide, The Red Cardinal Story Our final episode for Season 2 focuses on family, friends and holiday wishes. In this episode, Host Sherri...
2nd Annual Caregiver Holiday Gift Guide
Caregiving Club’s 2nd Annual Caregiver Wellness Holiday Gift Guide is here – just in time for Black Friday and Cyber Monday shopping. Check out Caregiver Wellness, Older Adult Wellness and Wellness for the Home ideas.
Season 2, Episode 18 – Show Notes and Resource Links
Thanksgiving Episode: Musical Menus with Professor Charles Spence, More National Family Caregiver Month, Gratitude Gravy Recipe In this episode, Host Sherri Snelling celebrates the Thanksgiving season along with November’s National Family Caregiver Month. Special...